
All pain in the legs on walking is not due to arthritis nor all non-healing wounds in the legs and feet are due to diabetes.
In fact, its far from the truth.
Pain in the legs on walking – and which is relieved by stopping the walk and resting ; is typically a pain due to a decrease in blood supply to the legs and feet. It’s called ‘Intermittent Claudication’, and is usually due to a blockage of the arteries supplying blood to the legs – Peripheral Arterial Occlusive Disease or Peripheral Arterial Disease.
What is Peripheral Artery Disease?
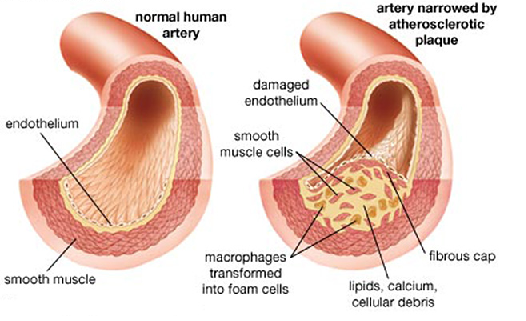
Peripheral Artery Disease (PAD) is also known as Peripheral Vascular Disease (PVD). It is usually caused by a process known as Atherosclerosis which results in thickening, hardening and narrowing of the arteries – tubes which supply blood from the heart to the various organs of the body.
PAD can occur in any blood vessel in the body. The common areas are the blood supply to the legs, the brain, the heart, the kidneys and the intestines. The heart accounts for only around 20 percent of cases of atherosclerosis.
What the common factors responsible for PAD ?
- Chronic Smoking,
- Uncontrolled Hypertension and Diabetes,
- High Cholesterol,
- Sedentary Life ( read as ‘LAZY’ lifestyle with absence of regular excercise) as well as a
- Positive Family History of similar disease, are very important ‘Risk-factors’ of PAD.
Control of these factors is important for any successful result after medical, interventional or surgical treatment.
Is Peripheral Artery Disease ‘Dangerous’ ?
Any disease untreated can be dangerous. And yes, PAD can be dangerous too. The complication depends on the region of the body in which blood supply is decreased or stopped.
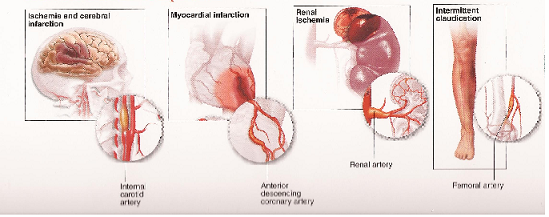
The results can be as follows:
1. The Legs : Leg pains on walking usually relieved by rest. Untreated this progressed to blackening (GANGRENE) of the toes and / or the foot/leg and may need an AMPUTATION.
2. The Brain : This may result in a range of complications from transient loss of consciousness to STROKE and PARALYSIS.
3. The Kidneys : This results usually in Kidney failure and may need Hemodialysis, and
4. The Intestines : This usually results in pain and a sensation of ‘Bloating’ in the abdomen after meals. This can even lead to GANGRENE of the intestines and may need the intestines to be removed.
Does all PAD need treatment ?
Yes and No.
Control of ‘Risk-Factors’ by exercises, diet modification, stoppage of smoking, and medications, is a part and parcel of any treatment of PAD. Specific Medications are required in some while surgery or interventional therapy is occasionally necessary to prevent a leg amputation.
Do all PAD have complications ?
No. Control of risk-factors is very important to prevent complications in PAD.
Are there any warning signs of the risk of complications in PAD ?
Yes.
The symptoms of PAD not relieved by control of risk factors is a definite signal that complications are likely. However, diabetics may not have any pain. Delayed healing or non-healing of leg wounds, loss of hair in the legs, friable toe/finger nails are signs of problems on their way.
Though PAD progresses over time at variable rates in each individual de¬pending on the area of circulation affected, the signs and symptoms of PAD may not arise until later in life. For many, the outward indications will not appear until the artery has narrowed by 60 percent or more.
Can PAD present suddenly ?
Yes.
Diabetics may not have any pain. Also a piece of cholesterol, calcium or blood clot may abruptly breakdown from the lining of the artery or a narrowed artery blocks off completely, blood flow will be totally obstructed and the organ supplied by that artery will suffer damage. In the limbs, it can result in a GANGRENE, if untreated.
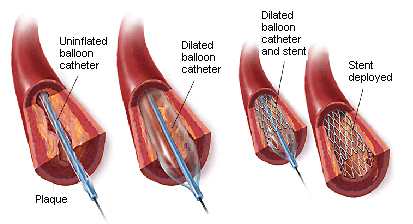
Therefore, it is usually recommended that when the narrowing in the blood vessels is more than 70 percent, some procedure to improve the blood supply – Revascularisation , is preferably done.
This may involve an angioplasty with or without stenting, an endarterectomy ( surgery to remove the plaques), a surgical bypass or even a combination (hybrid) procedure.
What are the tests needed to diagnose PAD ?
A Colour Doppler – a specialised ultrasound of the arteries, is usually the only test needed to confirm a clinical diagnosis of PAD.
In cases planned for angioplasty or bypass, an angiography is usually done to plan the correct procedure. The Angiogram is preferably done by a CT or a MRI scan, and involves an intravenous injection in the centre. This does not need hospital admission.
What decides the type of revascularisation : Angioplasty or Bypass ?
The length of the ‘blockages’ – long or short, their severity – total or sub-total, the number – single or multiple ; are the key factors deciding the type of procedure.
Additional factors to be considered are the general fitness of the patient, and unfortunately at times, the economic status of the patient.
Are treatments for PAD expensive ?
PAD procedures are highly specialised and complicated procedures .
They involve high quality equipments and materials. Sometimes, even costly artificial ‘graft’ materials and/or ‘stents’. Quality does come at some price but our packages are very just and cost effective. A ‘natural’ limb is anyways PRICELESS.

Are there any special differences in our treatments ?
Yes. To summarise in brief, we tend to do most procedures under regional anesthesia and not general anesthesia, use patient’s own veins for the bypasses and specialise in what are called as « Cross-Over » procedures in critical cases. The aim being to make the procedures not only safe and simple for the patient, but also to decrease his or her hospital stay and the costs !




